LGBTQ+ Adults with Parkinson Disease
Dr. McIsaac is recruiting for a qualitative study on the lived experiences regarding Healthcare access of people with Parkinson disease (PD) identifying as LGBTQ+, non-LGBTQ+ people with PD, care partners, and healthcare providers. The study will be looking to interview (by Zoom) people from across the U.S., from urban and rural areas and from across the socioeconomic spectrum.
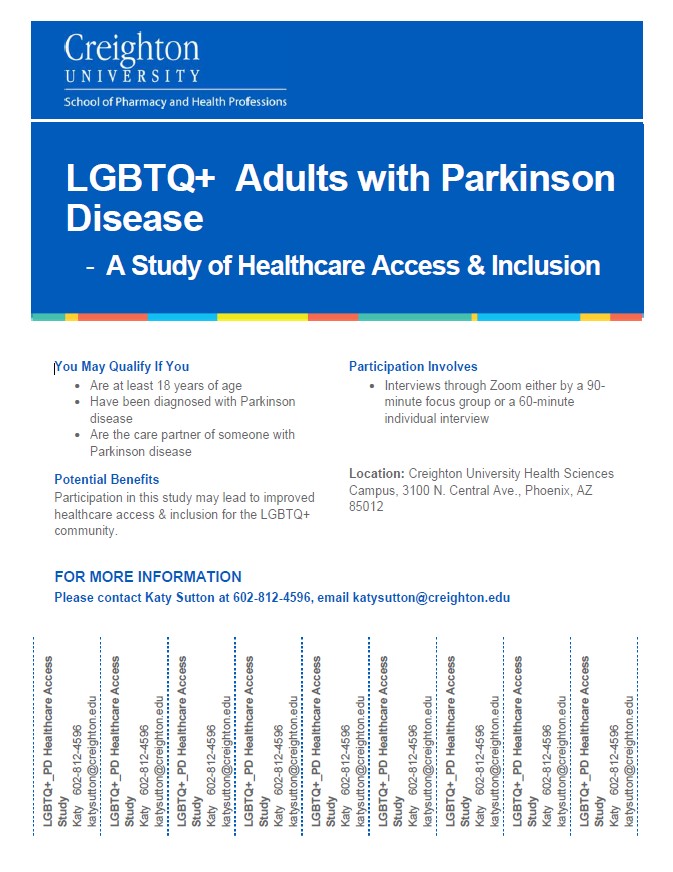
She is hoping that you can help spread the word about the study. Since people with PD who identify in the LGBTQ+ community is a much smaller group than all people with PD, we are prioritizing recruitment of LGBTQ+ people with PD first. She would be very grateful for your help to distribute this flier (click here) as widely as possible. You can contact her at taramcisaac@creighton.edu with questions or to chat further about the study. You can also find more information at our Clinicaltrials.gov study link (active) or in the study rationale below.
https://clinicaltrials.gov/ct2/show/NCT05502055?term=NCT05502055&draw=2&rank=1
Study Rationale
LGBTQ+ older adults overall face greater barriers to accessing and receiving healthcare and social support and have worse mental and physical health than non-LGBTQ+ older adults. Approximately 1 million adults in the U.S. live with PD1 and an estimated 3% of elders aged 55+ identify as LGBTQ+.2 Although relatively small in number (~30,000), information on the intersection of LGBTQ+ older adults and people living with PD is almost non-existent.
While there is virtually NO research on this population (LGBTQ+ with PD), research shows that experiences of LGBTQ+ adults over 60 regarding chronic disease management fall into three categories of health disparity: social support, health provisions, and aging resources.3 These disparities are related to lack of access to culturally appropriate care; social inequities and personal histories of discrimination, violence, and accumulated minority stress; mistrust, fear of and experienced discrimination by healthcare providers; and lack of social support and social isolation.4-8 The aging LGBTQ+ population is much less likely than their non-LGBTQ+ peers to have spouses or children for social support and more often rely on families of choice that are commonly their peers and thus also older, have health and function difficulties of their own, and with less legally recognized connections for navigating care institutions and systems.9
Healthcare and relationships with healthcare providers overall are negatively impacted for LGBTQ+ individuals by the limited education and knowledge healthcare providers have of the lives, experiences, and bodies of LGBTQ+ people whom they serve.9,10 A compounding issue is that LGBTQ+ elders are often afraid to disclose their sexual and gender minority status to their healthcare provider based on long histories with discrimination including abuses and mistreatments against LGBTQ+ people in medicine.11,12
The health disparities of LGBTQ+ individuals deepen with aging due to accumulated discrimination, inadequate understanding by healthcare providers of their life experiences and needs, and greater isolation. The added dimension of living with a complex neurodegenerative disorder such as PD, that impacts every aspect of one’s life, is unexplored in the literature. Our study on the perspectives of LGBTQ+ adults with PD, their care partners and healthcare providers, provides a unique opportunity to understand the intersections of gender and sexual minority status and disability as it relates to complex healthcare decision-making and system navigation.
References:
- Marras C, Beck JC, Bower JH, et al. Prevalence of Parkinson’s disease across North America. npj Parkinson's Disease. 2018/07/10 2018;4(1):21. doi:10.1038/s41531-018-0058-0
- Jones JM. LGBT Identification Rises to 5.6% in Latest U.S. Estimate. Gallup, Inc. Accessed April 18, 2021, https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx
- Nowakowski ACH, Chan AY, Miller JF, Sumerau JE. Illness Management in Older Lesbian, Gay, Bisexual, and Transgender Couples: A Review. Gerontol Geriatr Med. Jan-Dec 2019;5:1-10. doi:10.1177/2333721418822865
- Barrett N, Wholihan D. Providing Palliative Care to LGBTQ Patients. Nurs Clin North Am. Sep 2016;51(3):501-11. doi:10.1016/j.cnur.2016.05.001
- Caceres BA, Frank MO. Successful ageing in lesbian, gay and bisexual older people: a concept analysis. Int J Older People Nurs. Sep 2016;11(3):184-93. doi:10.1111/opn.12108
- Lottmann R. [Sexual and gender diversity and care for older people-intersectional perspectives and the relevance of situations and contexts]. European journal of geriatrics. May 2020;53(3):216-221. Sexuelle und geschlechtliche Vielfalt in der Altenhilfe - Intersektionale Perspektiven und die Relevanz von Situationen und Kontexten. doi:10.1007/s00391-020-01704-7
- Westwood S. The myth of 'older LGBT+' people: Research shortcomings and policy/practice implications for health/care provision. J Aging Stud. Dec 2020;55:100880. doi:10.1016/j.jaging.2020.100880
- Westwood S, Willis P, Fish J, et al. Older LGBT+ health inequalities in the UK: setting a research agenda. J Epidemiol Community Health. May 2020;74(5):408-411. doi:10.1136/jech-2019-213068
- Brennan-Ing M, Seidel L, Larson B, Karpiak SE. Social care networks and older LGBT adults: Challenges for the future. J Homosex. 2014;61(1):21-52. doi:10.1080/00918369.2013.835235
- Rosendale N, Ostendorf T, Evans DA, et al. American Academy of Neurology members' preparedness to treat sexual and gender minorities. Neurology. Jul 23 2019;93(4):159-166. doi:10.1212/wnl.0000000000007829
- Croghan CF, Moone RP, Olson AM. Friends, family, and caregiving among midlife and older lesbian, gay, bisexual, and transgender adults. J Homosex. 2014;61(1):79-102. doi:10.1080/00918369.2013.835238
- The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. . National Academies Press (US); 2011. https://www.ncbi.nlm.nih.gov/books/NBK64806/